My Story: The 10 people and groups that enabled me on my challenging breastfeeding journey
For World Breastfeeding Week, I’m sharing the story of my breastfeeding journey and the 10 people and groups that helped enable me to breastfeed my baby. May this help future mamas to build their village! Please feel free to share your story on what enabled you, what hindered you, what you think could have enabled you to breastfeed, or any other related thoughts.

on my breastfeeding journey
#WBW2019 #WABA #EmpowerParents #EnableBreastfeeding #breastfeeding #SDGs #worldbreastfeedingweek2019
Back in 1990, government representatives from 30 countries came together with international organizations including UNICEF and the World Health Organization (WHO) to protect, promote and support breastfeeding internationally. They reached agreement to do just that under the Innocenti Declaration of 1990. The global goal was that “all women should be enabled to practice exclusive breastfeeding” through development of national strategies for this, promoting a breastfeeding culture, improving nutrition of mothers, and implementing other key actions contained in the Declaration.
Every year since the Declaration was adopted, the World Alliance on Breastfeeding Action (WABA) has organized World Breastfeeding Week between August 1st – 7th. They continue working together with WHO, UNICEF and other agencies in the Global Breastfeeding Collective to highlight the continuing importance of breastfeeding for mothers, babies, families, the economy and society at large.
This year the theme of World Breastfeeding Week 2019 is “Empower Parents, Enable Breastfeeding.”
This got me thinking about what it was that empowered and enabled hubby and I to breastfeed our baby. She was breastfed for 11 months: the first 2.5 months with some formula supplementation, the next 3.5 months exclusively breastfed, and the following 5 months breast-milk was combined with a growing range of solid foods beginning from 6 months old.
One year on from being deep in the depths of – what was to me – a steep learning curve on breastfeeding, I am now able to reflect on the process and share some insights. Breastfeeding, it takes a village…!
My Village: The 10 people and groups that enabled me on my challenging breastfeeding journey
Here are the 10 people and groups (in roughly chronological order) that empowered and enabled me on my breastfeeding journey, even through my struggles to do so. What I learned through this experience is breastfeeding takes a village!
- Myself: My decision, mindset and motivation and my body, health and recovery process
- Baby: her health, interest and desire
- Hospital: Lactation support in the days after birth
- Hubby: his motivation, support and contributions
- Our Employers: Maternity leave, paternity leave, sick leave
- Family: Two sets of grandparents
- Local breastfeeding center: Lactation consultant
- Health Insurance Company: Coverage for lactation support
- Friends
- Our Nanny in Bangkok
1. Myself: Elements within and outwith my control
My decision and motivation to breastfeed (within my control)
The rational decision: Before the birth, I had spent time reading about some of the benefits of breastfeeding for the mother, the baby, employers, the environment and society as a whole. I was pretty convinced it made sense for me and my baby that I should choose to breastfeed – if I should be lucky enough to have the choice. I accepted I may not have the choice given various unknown health or other factors that may prevent breastfeeding, but if the choice was mine, I would breastfeed.
The social and cultural decision: I had been breastfed by my mother, most friends I knew were breastfeeding their child, and it was part of my social and cultural norms and expectations to breastfeed my own baby.
The emotional decision: I had heard of the wonderful connection that some mothers describe when breastfeeding due to rising hormones like oxytocin, and I wanted to experience that too. I also bought into the images shared in books and online of the new mother peacefully resting on a rocking chair with her sleeping baby in her arms after a breastfeeding session.
In reality this is not how it worked out for me, but so it goes with many aspects of parenting!
“What Mums Can Do”. Source: https://www.who.int/
After the Birth
After the birth, I encountered various challenges to breastfeeding (more below), yet I still was determined that I wanted to breastfeed. It wasn’t easy and while I wasn’t able to do so exclusively for the first 2 months, the efforts invested during that time paid off over the medium term and I was able to continue breastfeeding until the baby was 11 months old.
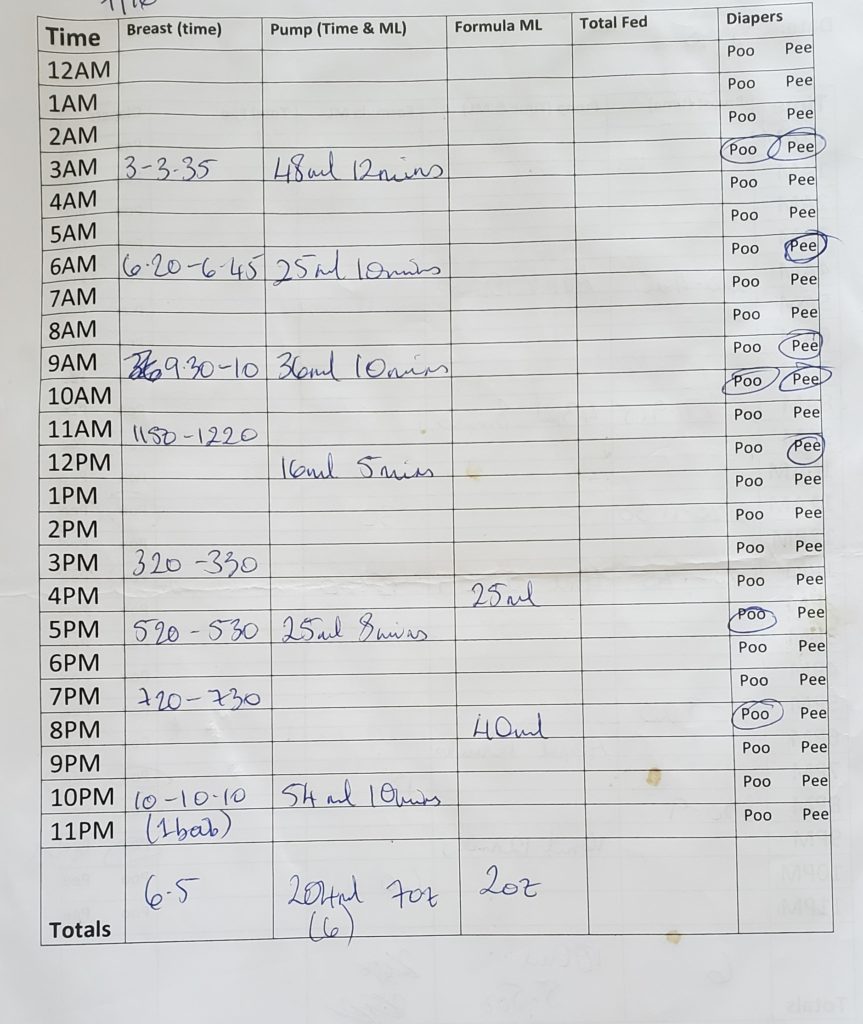
One of the ways I stayed motivated was through a chart that we kept each day (yes, she is my first baby!) where I could keep track of the amount of milk that I pumped and the amount of formula that was supplemented. Seeing the data, in the aggregate, change over the weeks to more and more pumped milk and less and less formula helped keep me motivated that all the effort was worth it. She was getting more milk from me (which in any amount is always a beneficial thing) and we were getting closer to transitioning away from formula.
My body, health and recovery for breastfeeding (outwith my control)
While I feel extremely fortunate to have had the birth that I wanted (vaginal delivery, no pain medications), the post-birth was another story and left my body traumatized. I experienced a ‘retained placenta‘, which is when the placenta attached to the uterus and does not come out naturally after the birth. As I was hemorrhaging pints of blood, I was asked whether I would like to go to the operating room under general anesthetic to have it removed, or continue with manual removal by the doctor while being awake with some intravenous pain medication. I was advised that the OR and general anesthesia option would delay my ability to begin breastfeeding since medication would be in the breast-milk (and transferred to the baby) and I wouldn’t be conscious enough to hold the baby safely. For this reason I opted to proceed with manual removal.
In the following hours after the procedure was completed, my body provided colostrum and thankfully my milk supply came in on the third day. The lactation consultants at the hospital seemed happy with the milk supply when I left to go home 5 days after the birth.
Baby is not gaining enough weight
However, two weeks after the birth the baby was weighed at her two-week check-up appointment and found to not have gained enough weight. Our pediatrician advised that there may be some constraints to the milk production given that my body had experienced some real trauma. In these situations, she explained that the body does what it can to protect and heal itself first, and only if there are resources and energy remaining does it produce milk for the baby. This is a very primordial survival technique and her explanation made sense to me.
Yet, I was so disappointed to hear that my body was not providing enough nourishment for our baby. It went right to the heart of what I saw my role as her mother to be – to grow her strong – and my body wasn’t able to do that. The doctor advised that we consult with a lactation consultant to help determine if there were any other issues affecting her ability to eat and gain weight (more on this below).
My milk supply was further hindered by the retained placenta that we believed to be fully removed, but were not entirely sure. In some circumstances where the placenta may not be completely successfully removed by a doctor, the body can think it is still pregnant and this slows milk production.
Recovering and boosting the milk supply
There were three ways to try and address this. First was an ultrasound to check that all the placenta had been successfully removed, which it had. Second was to try and rest to help accelerate my healing (good luck with that when you have a newborn, ha!). Third was to introduce a breast pump into my daily feeding routine with baby. This was designed to tell my body that not only was the milk it was currently producing not sufficient for my baby, but also to tell my body that I had twins and there were two babies needing milk! (A double breast pump can try to trick the body into thinking there is a baby at each breast).
All of this made the first 2-3 months of breastfeeding particularly challenging. But as more time passed since the birth, my body started to recover, it became stronger and adjusted to producing more milk via the pump, breastfeeding did get easier.
Managing other health conditions
Other health situations like the common flare-up of auto-immune condition after the end of the pregnancy meant that my doctor advised me not to breastfeed while on certain medications. I persisted on how important this was to me and we found alternative medications that managed to bring the condition under control again while still allowing me to breastfeed. In addition, contracting a bout of food poisoning while trying to breastfeed was challenging – I share my experience and techniques in 6 tips for breastfeeding when you have food poisoning.
2. Baby: her health, interest and ability to breastfeed

Baby always showed a strong interest in breastfeeding. She very much enjoyed being at the breast – perhaps a little too much though, as she tended to fall asleep there before eating enough. The lactation consultant at the hospital, and friends I spoke to who had faced a similar challenge, advised me to wake her up at the breast by taking her shirt off, spraying her feet with water and/or holding ice cubes to her toes.
It all sounded pretty tough to us but our neighbor with 4 kids also gave us this advice, and so we did them all. We needed a sense of humor about it though. We did have a laugh one 3am wake-up session about spraying her feet to get her to eat so often that we may end up training her, like Pavlov’s dog, to expect food to arrive every time she has wet feet in her childhood!
So her desire to be at the breast was clear, but what was less clear was the amount of milk that she was actually able to draw from the nipple. A lactation consultant evaluated her mouth and said she had both a tongue tie and a lip tie and that they should be released for her to be able to feed effectively.
Is it a tongue tie?
If so, that would mean a minor outpatient procedure of a surgical cut to the skin flap under the tongue and between the top lip and gum. She also mentioned that this was linked with autism. This statement is one sure-fired way to upset and worry a parent! Also, tongue ties are often over-diagnosed and are increasingly treated unnecessarily.
I wasn’t entirely convinced based on this one woman’s assessment, and so we scheduled an appointment with a pediatric ENT doctor. This doctor could perform the procedure there and then if it was deemed necessary. I made clear we just wanted an evaluation and it turned out her advice was that the baby, once she reaches 10 lbs in weight, should develop a strong enough jaw to create strong enough suction and repetition to be able to extract enough milk. Relief! No procedure required at that time. She was correct in her assessment, by the time baby reached 10 lbs (when she was about 2 months old), she was managing much better and I was reducing the number of pumping sessions I was doing per day.
So, again, time healed this issue thankfully.
It reminded me that the breastfeeding relationship between a mother and her baby is like a dance: it takes two to tango, it’s important to be in sync and you need to be reading what’s happening with your partner.
3. Hospital: Lactation support in the days after birth

As a first-time mother, I had no idea how to breastfeed. Yes, I read some articles, looked at some pictures and attended a class at our local breastfeeding center. But it’s just so different in real life! I found there was no substitute for hands-on support.
I wasn’t able to feed in the first hour after birth, as recommended, because of the procedure, but baby had skin-to-skin contact with her dad for a while as my placenta took a while to remove. It had been 80-90% attached making it a longer and more stressful process to remove than expected (normally a retained placenta is only about 10% attached), and I hemorrhaged around 6 pints of blood during that time.
We were fortunate enough to birth in a hospital in the US that does staff lactation consultants, one of whom came to visit me on the second day. Unfortunately, my baby was born on a Sunday morning and the lactation consultants don’t work weekends. But the midwife in the Labor and Delivery unit helped set us up with trying to breastfeed the first couple of times.

I did have to ask repeatedly for the lactation consultant to come and visit us, but when she was available, she was helpful. She showed me how to hand express some colostrum myself to give to the baby through a syringe. She provided a demonstration of different positions for feeding, one of which was the rugby hold, and proved to work best for us in the first weeks when baby wasn’t eating enough from the breast.
The risk of nipple confusion
What did really bother me about the hospital staff working with us was that they fed the baby formula from a bottle before I knew it was happening. When they took her to the nursery in the first evening, they fed her formula rather than bring her back to me to feed. I didn’t give consent to them feeding her formula, and my husband doesn’t remember doing so either. This is something that can undermine breastfeeding.
The morning that my milk came in, we had a bit of a stressful incident. The baby bit down on my nipple and I cried. It was stressful because my breasts felt very full and the nurse had brought baby back from the night nursery where she had (annoyingly to me) just fed the baby formula. So not surprisingly the baby was not hungry, yet my breasts were needing to be emptied. I wish I had known that I could ask for the baby to stay with me all night, or that even if baby had gone to the nursery, I could have asked for her to be brought back to my room during the night to feed.
However, at that point, making the best of a bad situation, the lactation consultant introduced the idea of expressing milk using a breast-pump and then feeding it to the baby via bottle. Bearing in mind though that it’s not recommended to introduce bottles to babies who are being breastfed. It creates a risk of what’s called ‘nipple confusion‘ that can cause the baby to reject the breast after bottle-feeding. She explained these risks but advised she believed it was still best that the baby get the milk by whichever means worked best in our situation, so we agreed.

We were also sent home with a supply of formula for baby as well as with a collection of bottles, teats and a breast pump rental.
In the end though, we were fortunate that our baby never developed nipple confusion. She happily went between the breast and the bottle with both expressed milk and formula.
4. Hubby: his motivation, support and contributions
His first contribution was standing by decisions I was making about whether to go to the OR or continue with the manual removal of the placenta. And from there on there are almost too many to list. But here goes…
When I wasn’t able to breastfeed in the first hour, he held the baby skin-to-skin. As we began our breastfeeding journey, he went to ask for the lactation consultant to come and show us how to breastfeed. He made sure I always had enough to drink and eat to keep energy up and aid milk production (staying hydrated is important). He lifted the baby from her hospital crib onto me to feed when I couldn’t stand or walk to get to her. And he tried to minimize the number of tests the nurses did on me during the nights in the hospital so I could try to get some rest.
When we got home, he re-arranged the bedroom so I could be next to baby and lift her out of her bassinet next to me for a breastfeeding session anytime. Washing all the breast pump parts several times a day was such a pain, and he did this without complaint or me asking. He came to every appointment with our lactation consultant, to the pediatrician and to the pediatric ENT for the tongue tie assessment. He took baby for her immunizations. He woke up for the night feedings to help keep baby awake, spraying water on her feet and rubbing her as I tried to feed her. And the supplemental nursing system was no joke (I hated that fiddly contraption), but still he helped me hook it up whenever we tried to use it.
I was feeding about 9 times a day, plus also pumping each time, and then supplementing with formula, which took up about 80% of my waking hours, so all other house chores fell to him.
He rocked. I know, particularly given my recovery situation, I could not have kept breastfeeding without his support and contributions. It was a real team effort.
5. Our employers: Maternity leave, paternity leave, sick leave
My maternity and sick leave
Coming from the UK where laws, norms and expectations are such that a mother can take up to one year of maternity leave, I was struggling with adapting to the idea that in the US there is no guaranteed maternity leave.

I worked for an international organization that allowed 3 months of maternity leave (14 weeks to be exact), and while this was definitely more generous than other friends received from their American employers, it still felt like such a short time. Only enough time to get baby to the end of the ‘fourth trimester’. It wasn’t enough time to get to the end of the WHO and UNICEF recommended 6 months of exclusive breastfeeding, which is what I was hoping, before the baby was born, to be able to do. (Once women return to work it is hard, though definitely do-able, as I do know many mothers who have done it, to keep a fixed schedule for using a breast-pump at work and storing milk to take home at the end of the day. Stress at work can also affect the let-down and the quantity of milk produced.
Nonetheless, it was necessary and helpful to have these 3 months of maternity leave to get over the toughest part of recovering from the birth, establishing breastfeeding and a steady supply of milk, and a (quasi) routine for baby. When I left the hospital to go home with my new baby, the furthest thing from my mind was what was happening in the office – and I believe many other new moms appreciate that too. Maternity leave allowed time to adjust to life as a new mother, to bond with the baby, and to set up some systems at home to adjust to our new modus operandi with a baby in the nest.
Every mother and baby is different – some mothers are keen to get back to work, some need the money, some prefer to be at home and are able to do so. Personally, I was not physically able nor would I have wanted to return to the office and leave my 1 or 2 month old baby in the care of someone else at that time. And I was very fortunate through my employer’s maternity leave policy that I didn’t have to do that, or to make a tough choice about my employment status.
As it turned out, I was put on short-term disability leave after the birth due to the severe complications, and my maternity leave did not begin until about 4 months after the birth. So I was able to spend the full 6 months at home with baby making our breastfeeding routine easier to keep to and more likely to be successful. Of course, no one wants to go through such a traumatic birth, but sadly it does happen to some of us, and what’s needed then is an employer who understands the need for recovery time and time with the baby. Leave policies in this regard is one of the most powerful attraction and retention benefits to younger talent working in this more modern, diverse workplace. It pays dividends in terms of loyalty and appreciation to the employer.
Hubby’s paternity leave, also known as ‘sick leave’
My husband wasn’t eligible for paternity leave with his American employer, but he did have a lot of sick leave saved up from almost 10 years of working with this organization.
I am going to call it paternity leave, because I believe we should just call a spade a spade. He requested the leave because he was expecting to become a new father, not because he was expecting to become sick or to take care of a sick baby.
I shared with my husband the experience of a colleague who had recently taken 10 weeks off work after the birth of his fourth child, and said that he found this the best way to do it, and he wished he had had the opportunity to do it that way with every previous birth. I didn’t ask my husband to take this amount of time off, but he decided himself that this is what he would ask of his employer.
As it happened, there were three other women in my husband’s unit at work who were pregnant all around the same time as I was. They did not have paid maternity leave available to them and so they requested 10 weeks of sick leave to recover from the birth and spend time with their baby. As it would be discriminatory on grounds of gender to give the sick leave to the woman and not the man to care for their child, my husband was granted 10 weeks sick (paternity) leave.
I’m extremely grateful that his employer granted him the 10 weeks of sick (paternity) leave as it would have been such a struggle without him home supporting me as I recovered, and the baby as she adjusted to life ‘on the outside’. I know that his presence at home was a major contributing factor to my ability to continue to breastfeed and I am thankful that he was with us for all the reasons mentioned above.
6. Family: Two sets of grandparents

Source: WHO: https://www.who.int/
My husband described the presence of the grandparents in our home helping with the baby as working like concentric circles. In the middle circle there was baby, then around that there was me, and around that was hubby, and around that were the grandparents. There was a sort of cascade approach to getting everything done to care for the baby, and for me as I recovered.
It was so helpful to have my own mother there to help me with breastfeeding – remembering to switch sides, helping keep it frequent, burping the baby between each breast, and giving me encouragement that we were doing well.
I was enabled to spend as much time as needed breastfeeding because there was so much support, at least for the first 4 weeks, by the two sets of grandparents who came to stay with us from out-of-state and out-of-country. They went to the supermarket, they did laundry, cooked, watched the baby and cleaned around the house while I breastfed and napped.
7. Local breastfeeding center: Our lactation consultant
In the city we lived in after the birth there are several great breastfeeding centers, and I feel fortunate to have lived in a community that has such helpful resources readily available. One such center is located near my employer at the time and I had become familiar with their space through going to various pre-birth classes on breast-feeding, breast-pumping, baby care basics etc. Being already familiar and comfortable with that environment, I called to schedule an appointment with one of their lactation consultants after our pediatrician advised that we have our breastfeeding situation reviewed.

An appointment can be done at the center, or alternatively, and often more helpfully for mothers with newborns, the consultants can come to your home.
Coming from the UK, where a health visitor comes to every new mothers home to help with breastfeeding and other baby-related questions, this is standard practice for me. It is also standard practice in the Netherlands as I highlighted in my book review of the The Happiest Kids in the World. But sadly in the US this is only available to those whose health insurance cover the cost of the consultant as well as the cost of their ‘visiting’ fee, or to those who can afford to pay out of their own pocket.
The lactation consultant we saw the first time was not what we had been hoping for and raised unnecessary alarm bells about the health of our baby. The second appointment we scheduled, we requested to meet with someone else. Fortunately, one of my friends who had recently finished breastfeeding recommended a very helpful and positive consultant.
With this consultant, we got on track with a schedule, tips, tools, techniques and advice to help us. This included supplementation with formula, potential for use of donor human milk, the supplemental nursing system, herbs (moringa, goats rue) etc. We did weigh-ins at every weekly visit for a couple of months and saw our baby’s weight grow. After a couple of months we stopped supplementing with formula. I felt we had progressed to our goal of exclusive breastfeeding and the lactation consultant at the breastfeeding center was definitely an enabling factor in my breastfeeding journey.
8. Health Insurance Company: Coverage for lactation support
In the US, any health insurance plan must cover the cost of a breast pump, but coverage to see a lactation consultant is more patchy. I felt lucky that the access I had to the expertise of these lactation consultants was covered under my health insurance. However, I don’t believe it should be down to feeling lucky – it should be available to any woman who wishes to consult a lactation specialist. Many countries in Europe offer these services as they understand the value it brings to the baby, mother, family, employer, economy and society in the longer term.
For me, it really was a game-changer in the way that I approached breastfeeding. It’s possible I may have given up early with the feeling that it’s just too burdensome, such a struggle and it wasn’t going well. It was very stressful and it would have been much easier for me to just take a step back and provide more formula. However, I believe the advice from the consultants helped me to try new things (some of which I enjoyed more than others!) and keep me in the game for as long as it took to establish a stable routine, get baby suctioning well and reach a sufficient milk supply.
9. Friends
Friends, particularly those who had recently been through the experience of learning to breastfeed, were really helpful to speak with. I had assumed, as many others, that “it’s such a natural thing and it will all come naturally to me”. There were so many things I had worried about, but breastfeeding had not been one of them. Yet it was reassuring to hear that it was not only me who had not just naturally been able to pull it off, the way that I had expected before baby was born. I really learned a lot from conversations with other friends who shared their breastfeeding journey with me.
I also appreciated the food they delivered for us that helped with my seemingly constant hunger! And their recommendations for great lactation consultants in the area.
10. Our Nanny in Bangkok
When the baby was 2.5 months old we packed up and headed overseas to visit family in the UK and then make a move to spend time living in Bangkok (here is my blog on adjusting to expat life with baby in Bangkok). One of the first things we did when we arrived in Bangkok was to interview for nannies to help care for the baby as my husband started his new job in the city. This was an interesting process in which I learned a lot, and shared my experiences and lessons in a previous post on how to find a hire a great nanny in Bangkok.
I’m so grateful we were able to hire a nanny to help us. While baby was now 3 months old, she was still breastfeeding throughout the night as well as during the day. We had managed to transition her from the formula supplements but I was still expressing milk through our breast pump. Man, those pump parts are a pain to clean, especially when there is no dishwasher in our Bangkok apartment! It was so helpful to have someone there with me to help with sterilizing the parts, and to take over other areas of running the household so I could still spend several hours a day breastfeeding.
It takes a village!
And this was the village that was kind enough, gracious enough and knowledgeable enough to help enable me through my breastfeeding journey.
I hope this was an insightful read and I would love to hear the breastfeeding journey’s of other mothers and babies. What was it that enabled you?
For this World Breastfeeding Week, please share your comments or stories that may help other future parents in their breastfeeding journey!


